You control your life, keratoconus does not. “We understand people react differently to the news they have Keratoconus. Lack of knowledge and support often creates fear. We recommend learning as much as you can about this condition and investigating the many options available to let you get back to your life.
While we believe it’s important to accept this diagnosis, we hope to help you realize there are many resources available to help you adapt.
Wondering why you can't just wear glasses or regular contact lenses?
During the early stages of keratoconus, standard eyeglasses or soft contact lenses can often provide patients with clear and comfortable vision.
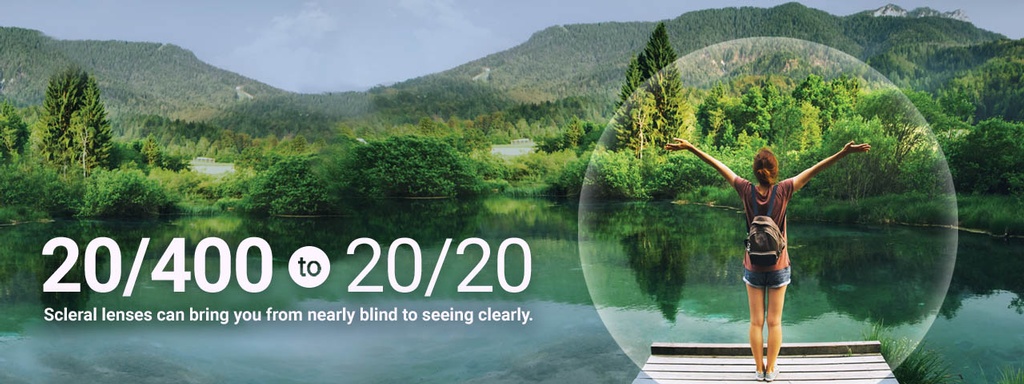
As the corneal shape becomes increasingly irregular, the eye becomes incapable of focusing light effectively. making simple tasks like reading, watching TV or driving very difficult. The distortion caused by keratoconus has been compared to viewing a street sign through your car windshield during a rainstorm.
When the cornea becomes highly irregular, eyeglasses or soft lenses cannot adequately compensate for the irregularities, which means they do not provide effective visual correction. Keratoconus that has progressed beyond the early stages needs to be treated with alternative visual correction.
Worried about the financial burden of Keratoconus?
We understand how much of a burden Keratoconus can be, financially and emotionally. We’re here to help and we have designed our care packages with this in heart and mind.
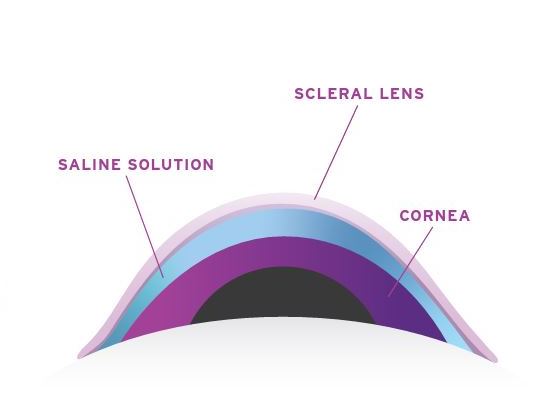
A large portion of the lifetime cost of keratoconus care is for the specially designed contact lenses that are required to correct the distorted vision caused by keratoconus. These lenses are more costly than contact lenses for routine vision correction, so we have to expect to pay more when visiting an eye care professional who provides Keratoconus contact lens fittings. You’re paying for the time involved in the fitting process, the special expertise, the equipment required to measure and determine the lens fit and the advanced type of lenses you’ll receive.
They require special handling by yourself, and special types of supplies. They require ongoing care and monitoring, and nothing about them is cheap. Scleral lenses are not something you want to adopt casually as a minor upgrade from other contact lenses. They are an investment and commitment.
Finding support within the Keratoconus community:
“Perhaps there is no better therapy than sharing your experiences with other Keratoconus patients. The mutual sharing of common experiences is both rewarding and assuring.”
- The Global Keratoconus Foundation: An organization dedicated to research and education about keratoconus. Click Here
- Living with Keratoconus Blog and Resources-Living with Keratoconus.com Click Here
- Keratoconus Group Blog- The largest community for keratoconus online. Provides stories and experiences of keratoconus patients.Click Here
- The National Keratoconus Foundation - Provides information to patients, newsletters, seminars and supports research into keratoconus. Click Here

What causes -inflammatory, progressive eye disorder affecting the anterior surface of the cornea. The cornea gradually thins, causing it to bulge into a cone-like irregular shape. Because the cornea is responsible for refracting most of the light that comes into the eye, any irregularity of the cornea can result in significant visual impairment, affecting the way they see the world.
It is this irregular distortion of the cornea that makes vision correction with glasses less than optimal. For this reason, other means of correcting vision are often necessary.
What causes Keratoconus?
Keratoconus most often appears in a person’s late teenage years; although it can been diagnosed in people in their forties and fifties.
The actual incidence of keratoconus is estimated to occur in 1 to 5 persons per 1,000 in the general population.
Keratoconus has no known geographical, gender, ethnic or social pattern…it occurs in all parts of the world.
The exact cause of keratoconus is not known; however, there are many theories on what may trigger this disease. It is important to note that no one theory provides a complete explanation, and it is likely that keratoconus is caused by a combination of things. It is believed that genetics, the environment, and the endocrine system all play a role in keratoconus…
- Genetics-One scientific theory is that keratoconus is genetic in origin. About 7% of patients have other family members with the disease. current research indicates that there is less than a one in ten chance that a blood relative of a keratoconic patient will have keratoconus.
- Environmental Factors-Keratoconus may also be associated with overexposure to ultraviolet rays from the sun, excessive eye rubbing, a history of poorly fit contact lenses and chronic eye irritation.
- Endocrine System-Another hypothesis is that the endocrine system (which dictates the release of hormones) may be involved, since keratoconus is often first diagnosed in adolescence
- Another view holds that keratoconus is a degenerative condition perhaps linked to the altered balance between enzymes and inhibitors within the cornea.
- Keratoconus may also be secondary to some disease processes.
(Information source-Menicon and KC.org)
What is Ectasia?
- Ectasia is defined as the expansion of body tissue, in this case the cornea which is the clear dome covering the colored part of the eye.
- The cornea’s primary responsibility is to focus light onto the retina to create clear, sharp vision.
- When the cornea thins, or becomes ectactic, it distorts the vision causing blur, multiple images, glare, haloes, dry eyes, light sensitivity and other undesirable visual phenomena.
What is Pellucid Marginal Degeneration?
PMD is a degenerative corneal condition, often confused with keratoconus.
- Pellucid corneas involve a larger distorted area than keratoconus. It is not unusual for 50% or more of the corneal surface to be involved. Because so much of the cornea can be affected, fitting this type of cornea can be quite challenging.
- It is typically characterized by the, thinning in the inferior and peripheral region of the cornea
- PMD typically presents bilaterally, although some cases affect only one eye.
- Typically presents in their 20’s.
- The cause of the disease remains unclear.
Intacs® corneal implants:
Intacs® are an FDA and Health Canada approved option for the keratoconus patient.
They are small crescents of a contact lens-like material (PMMA) that are implanted on the outer edge of the cornea by an Ophthalmologist.
One of the benefits to Intacs® in keratoconus is making the eye more tolerant to contact lenses, hopefully avoiding a corneal transplant.
More information can be found at >>IntactsforKeratoconus.com
Corneal Crosslinking:
- Corneal Collagen Crosslinking is a medical treatment that works by strengthening the corneal tissue by creating strong bonds (crosslinks) between corneal collagen fibers. Meaning…. CXL stabilizes the cornea and prevents the condition from worsening.
- The goal of the procedure is to prevent further progression of keratoconus or ectasia, not to correct or reverse the Keratoconus.
- Research indicates crosslinking can stop the progression of keratoconus but can also flatten the cornea potentially resulting in visual improvement.
- A patient with keratoconus who needed to wear contact lenses prior to CXL will likely still need to wear them after the treatment, but will hopefully experience less need to change the lens prescription.
While the exact cause of keratoconus has not yet been determined, research into keratoconus continues and new treatment options are continually under development…Hang in there!
More information can be found at >> Living with Keratoconus.com/cross-linking
Corneal Transplant:
As keratoconus progresses, some scarring of the cornea can occur. Eventually, contact lenses may no longer be a successful treatment. Instead, the cornea may need to be replaced surgically with a donor cornea of more regular shape. There are many different corneal transplant procedures available.